10% of patients with barrett esophagus will have adenocarcinoma at the time of initial diagnosis. Any degree of dysplasia in barrett�s esophagus is a risk factor for developing esophageal cancer (adenocarcinoma).

These cells may look a lot like cancer cells in some ways, but unlike cancer, they do not have the ability to spread all over your body.
Barretts esophagus with low grade dysplasia. 10% of patients with barrett esophagus will have adenocarcinoma at the time of initial diagnosis. Any degree of dysplasia in barrett�s esophagus is a risk factor for developing esophageal cancer (adenocarcinoma). The lifetime risk of esophageal cancer from barrett’s esophagus is low, probably on the order of 5% or less.
Longterm followup of patients with low grade dysplasia in barrett esophagus (sharma 2004) 10% progress to high grade dysplasia. [1] patients who have barrett�s esophagus with dysplasia may need more. Patients with barrett�s that do not have dysplasia may undergo an evaluation every one to two years.
10% of patients with barrett esophagus will have dysplasia. Rajesh krishnamoorthi from the mayo clinic reported at the american college of gastroenterology 2015 annual meeting, “barrett’s esophagus subjects with. If the barret’s esophagus is present but there is no evidence of precancerous changes are found in the cells, the patient will be diagnosed with no dysplasia.
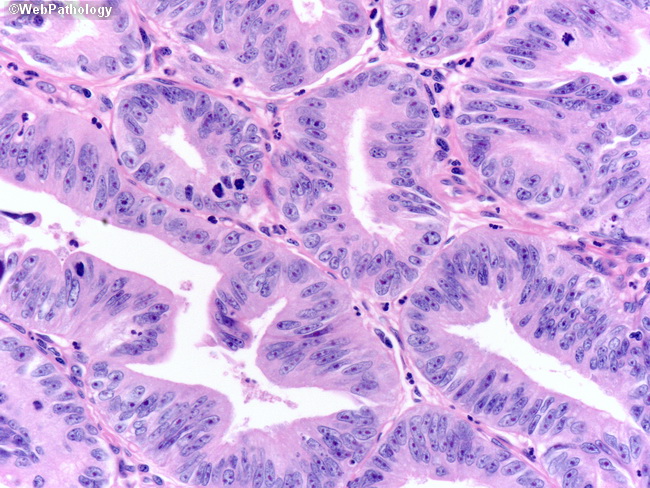
Although the risk of esophageal cancer is small, monitoring of barrett’s esophagus focuses on periodic exams to find precancerous esophagus cells. Closely packed overlapping basal nuclei with hyperchromasia and irregular contours, basal stratification of nuclei, and diminished goblet and columnar cell mucus (figure 2). 79 ( quiz 83.e1, 83.e3 ) :
In low grade dysplasia, epithelial abnormalities extend onto the mucosal surface. The nuclei appear hyperchromatic, elongated, stratified, crowded, and may display loss of mucin production. Images of phenotypes of dysplasia in barrett�s esophagus the second pattern consists of cells on the mucosal surface with obviously dysplastic nuclei (large, hyperchromatic, irregular contours) that are basally located in the cell with minimal or no.
So what if you do have high grade dysplasia (hgd)? Dysplasia describes how abnormal cells look. Surveillance programs with regular upper endoscopy seem to help detect dysplasia before it progresses to cancer.
For patients with no dysplasia, a periodic endoscopy to monitor the cells in the esophagus will be required. Diagnosis and grading of barrett esophagus related dysplasia can be challenging, especially with coexisting inflammation (hum pathol 1988;19:166) both low grade dysplasia and high grade dysplasia managed by endoscopic therapy, per the latest american college of gastroenterology (acg) guidelines (am j gastroenterol 2016;111:30) The risk of developing esophageal cancer increases if dysplasia is detected on esophageal biopsy.
Dysplasia increases the risk of developing esophageal cancer. The best practices outlined in this review are based on relevant publications, including systematic reviews and expert opinion (when applicable). Although the risk of esophageal cancer is small, monitoring of barrett’s esophagus focuses on periodic exams to find precancerous esophagus cells.
Pathologists can diagnose and grade dysplasia by looking at esophageal biopsies under the microscope. People with barrett�s esophagus have a higher risk of developing abnormal cells, called dysplasia. Radiofrequency ablation (rfa) has been shown to be an effective treatment for lgd in clinical trials but.
These cells may look a lot like cancer cells in some ways, but unlike cancer, they do not have the ability to spread all over your body. 1 however, there is considerable.